Patients with end-stage renal disease who are unable or are waiting to receive a transplant rely on dialysis for life saving care. Dialysis replaces the role of the kidneys by removing waste products and excess fluid. Fluid overload is a common consequence as hemodialysis patients struggle to limit sodium and fluid consumption, making it difficult for intermittent dialysis to keep up.
In addition, protein-energy malnutrition and low albumin levels can contribute to challenges with fluid removal that many patients experience. With the right nutrition and diet counseling, this could be avoided.
Albumin provides 80% of the colloid osmotic pressure in the plasma. That pressure keeps fluid in circulation and if it decreases it leads to more fluid equilibration between the plasma and other fluid compartments.
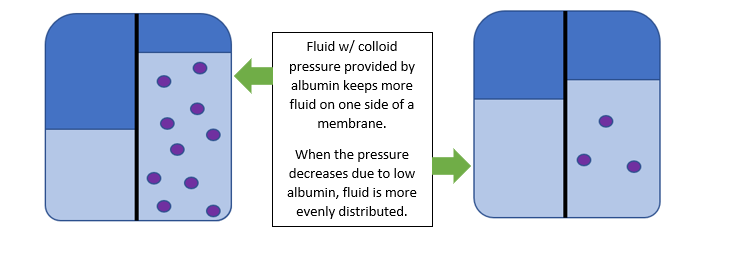
Without proper vascular pressure, fluid shifts out of the plasma space, the dynamics of fluid removal during dialysis will change and make it more difficult for patients to reach euvolemia. This is because dialysis draws fluid directly from the plasma, with more fluid residing outside of the plasma more time has to be allowed for plasma refill.
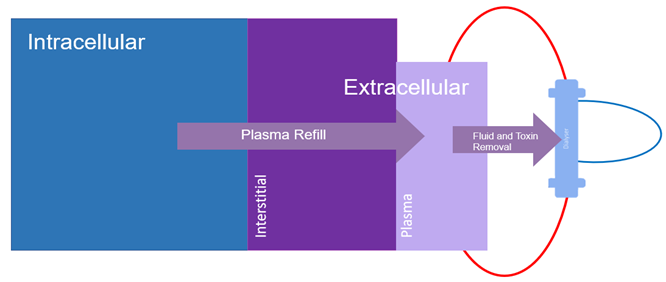
This is why ultrafiltration rates should not exceed 10-13ml/kg/hr as higher rates do not allow adequate time for the plasma to refill.
To improve oncotic pressure and plasma refilling, John et al identified that improving albumin levels may help. There are many ways to achieve improved albumin in dialysis patients including counseling patients to increase dietary protein intake of both animal and plant-based proteins, providing oral nutrition supplements with concentrated amounts of protein, and adding intradialytic parenteral nutrition (IDPN) for HD and intraperitoneal nutrition (IPN) for PD during the dialysis session.
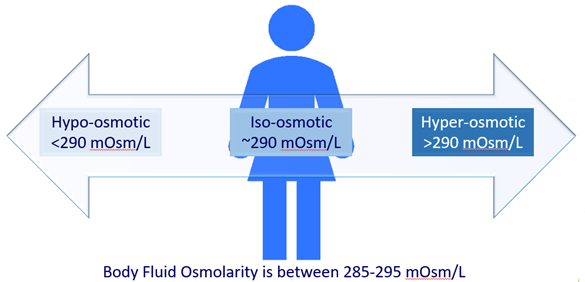
IDPN has the potential to further improve plasma refill rate due to the hyperosmotic nature of the therapy. Similar to the way normal saline has been used to treat patients with hypotension to quickly move fluid into the plasma, amino acids provide similar hyperosmotic pull as fluid likes to move where there is a higher concentration of solutes.
To learn more about protein status and the potential benefit of IDPN and IPN therapies for dialysis patients, check out the below resources:
- Article Spotlight: Malnutrition, inflammation, and fluid overload and their association with hemodialysis patient survival
- IDPN Upgrade
- Clinician Perspectives on IDPN
- PCA’s Clinician Log-in for patient and clinician resources
References
- Kooman, J. P., & van der Sande, F. M. (2019). Body fluids in end-stage renal disease: statics and dynamics. Blood Purification, 47(1-3), 223-229.
- John, B., Tan, B. K., Dainty, S., Spanel, P., Smith, D., & Davies, S. J. (2010). Plasma volume, albumin, and fluid status in peritoneal dialysis patients. Clinical Journal of the American Society of Nephrology, 5(8), 1463-1470.
- Shah, M. M., & Mandiga, P. (2019). Physiology, Plasma Osmolality and Oncotic Pressure.
- Pupim, L. B., Flakoll, P. J., & Ikizler, T. A. (2004). Nutritional supplementation acutely increases albumin fractional synthetic rate in chronic hemodialysis patients. Journal of the American Society of Nephrology, 15(7), 1920-1926.
- Mason, A. K., Malik, A., & Ginglen, J. G. (2019). Hypertonic Fluids. In StatPearls [Internet]. StatPearls Publishing.
- Hecking, M., Moissl, U., Genser, B., Rayner, H., Dasgupta, I., Stuard, S., … & Port, F. K. (2018). Greater fluid overload and lower interdialytic weight gain are independently associated with mortality in a large international hemodialysis population. Nephrology Dialysis Transplantation, 33(10), 1832-1842.
- Pinter, J., Chazot, C., Stuard, S., Moissl, U., & Canaud,
