
As a Registered Dietitian Nutritionist (RDN), I had the pleasure of working with people on dialysis for many years. During this time, I witnessed
many success stories for my patients on hemodialysis (HD) with intradialytic parenteral nutrition (IDPN). However, it was not until I began working
with Patient Care America, where I collaborate with fellow RDNs to help them access dialysis-specific nutrition support for malnourished patients, that I got
to hear of the remarkable outcomes that are possible for patients on peritoneal dialysis (PD) using intraperitoneal nutrition (IPN) therapy.
As many of us reading this blog may already know, living with chronic kidney disease (CKD) and undergoing dialysis can be a difficult journey filled
with many challenges. Despite these challenges, there are stories of success that inspire hope.
One example is the story of a PD patient who found a renewed sense of strength and vitality through the integration of IPN therapy into
her treatment regimen.
This patient was diagnosed with CKD several years ago. As her condition progressed, she started on in-center hemodialysis (ICHD) but eventually transitioned to PD, a form of home-based renal replacement therapy. PD is associated with certain benefits when compared to ICHD including:
- Better 5-year survival rates
- Lower prevalence of mild cognitive impairment
- More consistent removal of toxins due to less wait time between treatments
- Lower cost per-patient-per-year
- Increased independence and improved quality of life
However, many PD patients encounter problems like fatigue, a decrease in appetite along with early satiety, reduced spontaneous intake of protein,
and GI issues. This can lead to the development of malnutrition and protein energy wasting (PEW), as observed in this patient. Initially her PEW manifested in the in the loss of lean body mass, which accounted for her fatigue and was attributed to reduced intake of nutrition due to early satiety.
Despite the challenges, she was determined to improve her quality of life. Embracing the recommendations from her Registered Dietitian Nutritionist (RDN), she diligently increased her consumption of protein-rich foods and explored oral nutrition supplements provided by her clinic. However, when her condition showed no signs of improvement, her RDN suggested incorporating IPN therapy into her PD regimen. IPN therapy provides a customized amino acid solution that is infused directly into the peritoneal cavity in place of a conventional dextrose-based PD solution. Once infused, the amino acids are absorbed by the body, providing essential protein and calories while still providing the necessary ultrafiltration and removing unwanted toxins.Patients receiving IPN often see improvement in their albumin levels. In fact, a cohort from a 2021 analysis of malnourished patients referred by dietitians and PD nurses
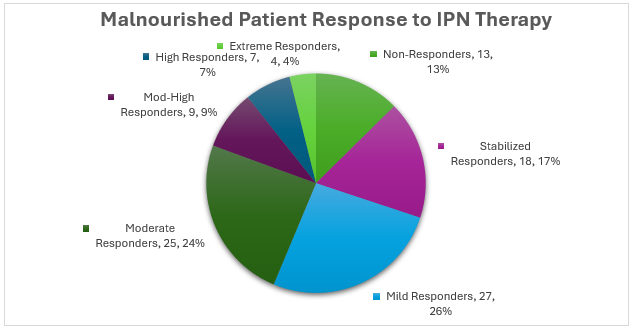
and started on IPN therapy with Patient Care America showed varying and overall positive responses to therapy. Patients were referred for albumin <3.5g/dL, which is another indicator of malnutrition and possible PEW, and showed a response rate of 87%. Response rate was broken down into incremental improvements of 0.2g/dL which is considered clinically meaningful. 17% of patients stabilized on therapy, meaning their albumin stopped declining.
More importantly, 70% saw an improvement in albumin anywhere from 0.2g/dL to >1.0g/dL.
But what does an increased albumin really mean for the patient’s day to day life?
In this patient’s case, with guidance from her interdisciplinary team and PCAs Clinical Support Nurse to diligently embrace IPN as part of her daily
PD regimen, she saw very positive real-life changes.
Her response was almost instantaneous as she noticed significant improvements in her overall health and well-being.
Could we talk further on how the patient felt before the therapy to build on what “feeling really good” means?
One of the best emails I’ve received since working with PCA was an email from the patient’s RD telling me how great the patient looked when she saw her, and how she has been reporting “feeling really good!”
The IPN therapy was helping to provide her body with the necessary nutrients to combat muscle wasting and fatigue, which was allowing her to regain strength and energy. She now looks forward to seeing her RD and the rest of the team at her clinic visit each month to discuss her progress.
By embracing this therapy, she encountered the benefits often associated with IPN therapy, becoming a beacon of inspiration for other patients confronting similar challenges. Her journey reminds us what can be achieved when patients and healthcare providers work together towards a common goal:
improving quality of life and fostering wellness despite adversity.
To learn more about Patient Care America’s IDPN and IPN therapies for malnourished patients on dialysis visit pcacorp.com and our Clinician Portal.
We thank our guest blogger Kerri Beck, RDN, CDN, for sharing her knowledge and writing this blog post!

