
September is Malnutrition Awareness Month, and as Renal Dietitians we understand that the nutritional assessment of dialysis patients is among the most complex of any disease state.
Bioimpedance Analysis (BIA) has gained traction as a valuable tool for assessing fluid balance and nutritional status. While BIA offers valuable insights
into body composition and fluid distribution, offering a non-invasive, quick, and relatively easy way to assess a patient’s nutritional status, it is crucial
to recognize its challenges and limitations for dialysis patients. Understanding these can help healthcare professionals make informed decisions about integrating BIA into patient care.
Understanding Bioimpedance Analysis (BIA)
Bioimpedance Analysis (BIA) measures the electrical impedance of body tissues by passing a small, harmless electrical current through the body.
This technique provides information about body fluid compartments and composition, such as lean body mass and body fat percentage.
Although BIA can offer useful data, it is important to be aware of the potential pitfalls and considerations involved.
Challenges and Limitations of BIA for Dialysis Patients
- Accuracy Concerns
The accuracy of BIA can be affected by various factors, which may impact the reliability of the measurements:- Hydration Status: BIA relies on the distribution of water in the body. Variations in hydration status, such as being over-hydrated
or under-hydrated, can skew results and lead to inaccurate assessments of fluid status. - Body Position and Protocol: The accuracy of BIA can be influenced by the patient’s body position and adherence to testing protocols.
Variations in how and when the measurement is taken can result in inconsistent results.
- Hydration Status: BIA relies on the distribution of water in the body. Variations in hydration status, such as being over-hydrated
- Technical Limitations
While BIA devices are generally user-friendly, technical limitations can affect their effectiveness:- Calibration Issues: BIA devices require regular calibration to maintain accuracy. Inadequate calibration or maintenance can lead to erroneous data and misinterpretation of patient conditions.
- Device Variability: Different BIA devices may use varying algorithms and measurement techniques, which can result in differences in data interpretation and comparisons.
- Integration with Other Measures
BIA should be integrated with other clinical assessments for a comprehensive evaluation:- Complementary Use: BIA results should not be used in isolation. They need to be complemented with other diagnostic tools and clinical evaluations to ensure a well-rounded understanding of the patient’s health status. Common screening tools like the 7-Point Subjective Global Assessment (SGA) and the Malnutrition Inflammation Score (MIS) are valid and reliable tools for assessing nutrition status in dialysis patients.
- Data Interpretation: The interpretation of BIA data can be complex and requires an understanding of how the results fit within the broader context of the patient’s clinical picture.
- Patient-Specific Variability
Individual patient factors can influence BIA outcomes:- Variability in Body Composition: Patients with significant deviations in body composition from the norm, such as those with obesity
or edema, may have less accurate or less reliable BIA measurements. - Health Conditions: Underlying health conditions, such as diabetes or cardiovascular issues, can affect fluid distribution and body composition, potentially impacting the accuracy of BIA assessments.
- Variability in Body Composition: Patients with significant deviations in body composition from the norm, such as those with obesity
- Impact on Patient Experience
The use of BIA can have implications for patient experience:- Patient Compliance: Patients may experience discomfort or inconvenience due to the BIA testing process. Ensuring patient comfort
and compliance is essential for obtaining accurate measurements. - Misinterpretation of Results: If patients or healthcare providers misunderstand the results or the limitations of BIA, it can lead to inappropriate treatment decisions or heightened anxiety.
- Patient Compliance: Patients may experience discomfort or inconvenience due to the BIA testing process. Ensuring patient comfort
Addressing the Challenges
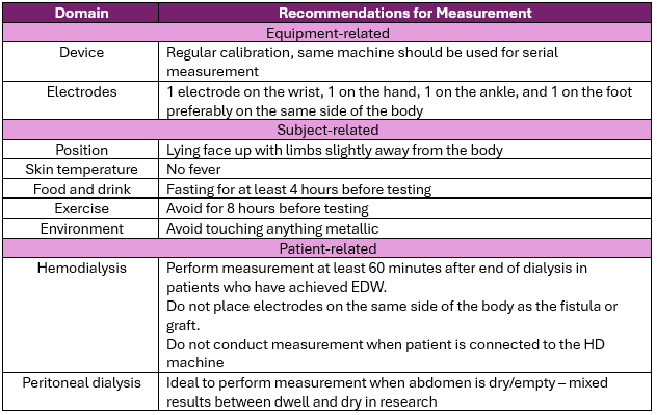
In 2023, Ng et al published a review of the use of BIA in dialysis patients which includes an outline of best practices for using BIA to more accurately assess body composition and nutrition status in dialysis patients:
In addition, clinicians can consider the following strategies:
- Ensure Proper Training and Calibration
- Regular Training: Provide ongoing training for healthcare professionals on the proper use of BIA equipment and interpretation of results.
- Integrate with Comprehensive Care
- Holistic Approach: Use BIA as part of a broader diagnostic and monitoring approach, combining it with other assessments and clinical data.
- Contextual Analysis: Interpret BIA results within the context of other clinical findings and patient-specific factors.
- Educate and Support Patients
- Patient Education: Educate patients about the purpose of BIA and how to prepare for accurate measurements. Address any concerns
they may have to improve compliance and comfort. - Clear Communication: Clearly communicate the limitations of BIA results and how they fit into the overall management plan.
- Patient Education: Educate patients about the purpose of BIA and how to prepare for accurate measurements. Address any concerns
While Bioimpedance Analysis (BIA) offers valuable information for managing dialysis patients, it is not without its challenges. By acknowledging
the limitations and addressing potential issues, healthcare professionals can use BIA more effectively and ensure that it complements a comprehensive approach to patient care. Balancing the benefits with an understanding of its constraints will help improve patient outcomes and support better nutrition management of dialysis patients.
To explore PCA’s available tools for assessing nutritional status and diagnosing malnutrition, visit our clinician portal, where you can also access
our 7-Point SGA training video.
Reference:
Journal of Nutrition Care. Bioimpedance analysis in patients with chronic kidney disease. Volume 49, Issue 3. September 2023, Pages 147-157.
Ng, J. K. C., Lau, S. L. F., Chan, G. C. K., Tian, N., & Li, P. K. T. (2023). Nutritional Assessments by Bioimpedance Technique in Dialysis Patients. Nutrients, 16(1), 15.

