
This year marks my 29th year as a registered dietitian. Prior to my current role with Patient Care America as a nutrition therapy consultant I spent 18 years in dialysis and most of my career was built on using the traditional interviewing method which I refer to as the “fix it method.” I had not heard of motivational interviewing (MI) until my company introduced an initiative to implement a new program for RDs.
I have to admit, when I heard about MI I thought to myself, “What’s wrong with the way I work with my patients?” The idea of MI was so foreign to me, and I found myself reverting to my old style. I struggled with it but kept up with my mentoring sessions and then something happened… I was approached to become a MI mentor which for me carried some benefits, so I decided to give it a shot!
My first attempt at mentoring was a complete fail! I felt discouraged but then with more practice I started to get the hang of it. I noticed that when I practiced with patients many of them opened up and I learned so much about them and their dialysis journeys. Miracles didn’t happen overnight, but the doors were starting to open!
Here are some thoughts to consider if you’re wondering if MI could be useful in your practice:
- Adherence to renal diet is as low as 31.5%
- 30-40% of patients on ICHD do not adhere to their treatment regimen
- Mild cognitive impairment and depression can negatively impact motivation
Yep, I get it – we are facing some serious challenges here…so how do we improve patient outcomes?
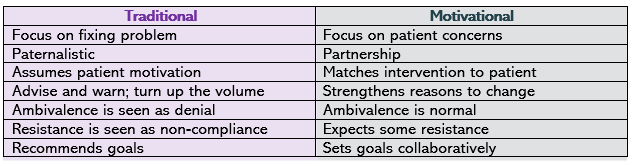
Let’s look at Traditional vs. Motivational Interviewing:
Studies show using MI even in short sessions with patients can:
- Reduce patient symptoms of anxiety, depression and sleep disorders
- Improve social functioning
- Improve dialysis attendance
- Reduce frequency of shortened treatments
- Produce more favorable phosphorus and albumin levels
These are tremendous benefits for patients and we have the tools to get there!
Here are some language skills to start building on, otherwise known as OARS:
- Open-ended questions
- Affirmations
- Reflections
- Summaries
I can remember trying this out and getting “stuck.” I would ask questions and not know where to go next. In time, it gave me guidance on how to approach patients who I could make progress with and were resistant to change. MI can reduce negative tension that builds up between clinicians and patients.
This is HUGE!
Some final thoughts:
Practice makes permanent! Try picking 1 or 2 skills at a time to work on. Keep up with training, mentoring, evaluations and feedback. Working on improving MI skills can be challenging and rewarding. Remember: focusing on collaboration puts the ownership on the patient NOT the RD!

We thank our guest blogger Kathryn Collins RDN, CSR Nutrition Therapy Consultant for sharing her knowledge and writing this blog post!
